Fed is Best Safe Newborn Feeding Guidelines
Given what we know about the risks of newborn hypoglycemia, hypernatremia, and hyperbilirubinemia, we have developed our guidelines based on the most conservative thresholds to protect the brain development of infants. The overall goal is to minimize unsafe levels of underfeeding, meet the newborn’s daily caloric requirement if persistent hunger or feeding complications occur, and maintain glucose, sodium and bilirubin levels at safe levels based on long-term outcomes data. We recommend the following:
- Follow the Pediatric Endocrine Society (PES) hypoglycemia thresholds no lower than 50 mg/dL at < 48 hours and no lower than 60 mg/dL thereafter. Feed breast milk, donor breast milk and/or formula to satisfaction and/or provide IV glucose to maintain levels above these thresholds for infants who are too weak or lethargic to feed.
- Perform glucose checks on exclusively breastfed newborns with point-of-care testing (POCT) and other newborns who are not being fed to satisfaction; send confirmatory laboratory glucose test if a newborn has a normal or borderline glucose level but treat immediate if POCT is low below 50 mg/dL.
- within 3 hours after birth [1] (which helps detect the infants at risk of developing early unsafe glucose levels due to low caloric reserve) and,
- every 6 hours thereafter until discharge [2] or until lactogenesis II has occurred, or when a newborn is being fed their full milk requirement with breast milk, formula, or both, and are not losing weight.
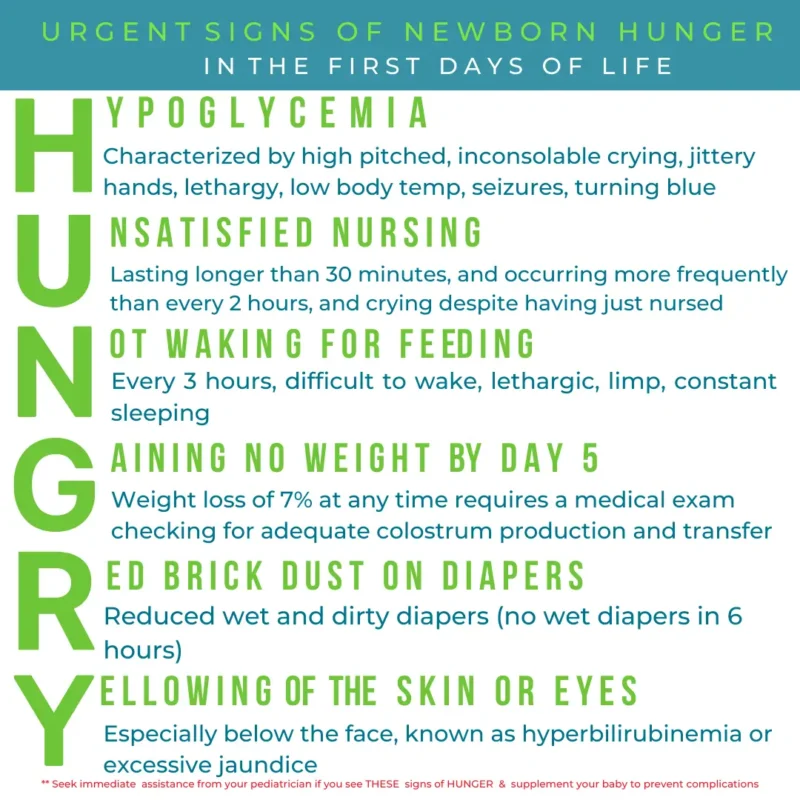
- for any signs of hypoglycemia or persistent hunger (see HUNGRY signs); send laboratory glucose tests if normal or borderline, along with electrolytes and bilirubin.
- If hypoglycemic, feed first to satisfaction if the baby is alert enough, STAT (as soon as humanly possible) – If hypoglycemia is identified, urgent restoration and stabilization of normal blood glucose with glucose provided by feeding or intravenous glucose is required to prevent ongoing injury to the brain due to low energy availability.
- Research has shown that colostrum has fewer calories than mature breast milk or formula and has been shown to have little effect on blood glucose levels.[3],[4] Antenatally expressed colostrum (collected before birth) fed as a supplement has also not been shown to be effective at preventing or treating hypoglycemia.[5]
- If lactogenesis II has not occurred, feed first with the most readily available safe method of supplementation, either banked donor breast milk or formula with a confirmed caloric content of 20 kcal/oz to satisfaction, within minutes of diagnosis to provide the calories needed to stabilize blood glucose.
- Calculate the daily caloric requirement per body weight (5.5 oz/kg/day) to help guide the volume of expressed and donor breast milk and/or formula feeds required to maintain normal glucose levels. Divide this amount by 8 feeds and feed the calculated volume every 3 hours or more frequently on demand. Correcting hypoglycemia is far more important to an infant’s brain than limiting formula supplementation or preserving exclusive human milk feeding status.
- Avoid high bilirubin and high sodium levels with adequate feeding – both high bilirubin levels and high sodium levels can be reduced by ensuring the infant is receiving their full milk requirement of 2.5–2.7 oz/lb/day or 5.5–6 oz/kg/day divided by 8–10 feeds. Once they have reached bilirubin levels of around 13 mg/dL or are in or above the high-intermediate risk zone on the bilirubin nomogram, or their sodium level has reached 145 mEq/L, then there is clear justification for full feeding with mother’s own breast milk, expressed breast milk, banked donor milk, and/or formula. Any safe infant milk will reduce these levels and protect an infant’s brain and their development. Treatment can include phototherapy for jaundice and/or careful correction of sodium through IV fluids done by a specialist.
- Evaluate breastfeeding and breast milk/colostrum supply and optimize breastfeeding while treating hypoglycemia – Manually express or pump with a hospital grade double electric pump to check for the presence of colostrum or mature breast milk and to measure milk volumes. Ensure maximum expression of breasts at least every 3 hours to maintain stimulus for milk production. If lactogenesis II has not occurred and milk supply does not provide the calculated full caloric requirement (0.7 oz/kg feed every 3 hours to a total of 5.5 oz/kg/day), then supplement hypoglycemic newborns with expressed breast milk, banked donor milk and/or formula to satisfaction until blood glucose levels are stabilized.
- For infants who are lethargic, too sleepy to feed, or have severe symptomatic hypoglycemia (seizures, abnormal breathing), IV glucose is needed to maintain normal glucose levels until the baby is alert enough to transition to oral feeding. Then feed the full milk requirement once stable while withdrawing IV glucose.
- Parents should be provided comprehensive instructions on criteria for supplementation at home before discharge, especially if milk has not come in – If signs of hypoglycemia or HUNGRY signs occur at home, and lactogenesis II has not occurred, parents should supplement until satisfied (about 60 mL) and seek immediate medical attention. If seizures occur or the baby cannot be woken, call 911 immediately.
- For health professionals: Avoid rapid correction and overcorrection of glucose – overcorrection of glucose levels (>150 mg/dL, >8.3 mmol/L) has also been shown to result in worse neurodevelopmental outcomes. [6],[7] It has been suggested that hypoglycemia may be more safely corrected by starting the glucose infusion without the initial bolus of glucose although randomized controlled trials have not yet been done to confirm this.[8] One study showed that keeping glucose levels between 54–72 mg/dL may prevent neurodevelopmental impairments associated with under correction and overcorrection.[9] Neonatologists stabilize glucose levels by carefully titrating the glucose infusion rate and frequently checking glucose levels to avoid abnormally low and high glucose levels.
Want to learn more about this topic?
Do you want to learn more about breastfeeding while ensuring safe and adequate feeding?
Dr. Christie and board-certified lactation consultant Lynnette Hafken have just released the online Fed Is Best Breastfeeding Course, where they discuss all the things that you will not hear from a breastfeeding book or class. In it they include secret tips and tricks that you normally have to pay hundreds of dollars to learn about, for the same cost of a hospital breastfeeding class. Click below to get in on the training!
Note to mobile users: The following table is best viewed in landscape or horizontal mode.
Health Professional Monitoring for Adequate Feeding
| Recommended Monitoring | Abnormal values | |
|
Weight |
Every 12 hours until weight loss ceases due to onset of lactogenesis II and/or full milk feeding to satisfaction with breast milk, formula, or both (can also be tracked with a home scale). |
>7% of birth weight or >75%ile on the NEWT™ nomogram |
|
Glucose |
Universal monitoring within 3 hours of birth to identify infants with the lowest caloric reserve glucose checks for prolonged or frequent crying or nursing, for signs of persistent hunger, along with other signs of hypoglycemia. |
Lower than 50 mg/dL in the first 48 hours Lower than 60 mg/dL after 48 hours |
|
Ketones |
Newer studies suggest that measurement of beta-hydroxybutyrate once daily during weight and/or bilirubin checks is helpful in assessing inadequate milk intake. |
>1.55 mmol/L is predictive of excessive weight loss >1.8 mmol/L is predictive of hypernatremic dehydration |
|
Sodium |
Can be measured with bilirubin and/or glucose checks, esp. for signs of persistent hunger with ≥5-7% weight loss. Should be checked for >7% weight loss. |
>145 mmol/L >150 mmol/L is associated with higher risk of developmental delay, requires careful correction with IV fluids (no greater than 0.5 mEq/hr) |
|
Bilirubin |
Per AAP guidelines: clinical assessment for jaundice every 8–12 hours and bilirubin checks for jaundiced newborns with non-invasive vs. blood tests. Closer bilirubin monitoring if jaundice difficult to assess due to skin tone. Supplementation before reaching phototherapy-requiring levels may prevent need for phototherapy. |
High-intermediate or high-risk levels per the Bilirubin nomogram. >13.5 mg/dL associated with developmental delay >19–20 mg/dL associated with serum markers of brain injury and higher risk of long term cognitive, academic, and developmental impairments |
|
Wet and dirty diapers |
Parents to check diapers before each feed. Newborns receiving the full milk requirement of 5.5 oz/kg/day will produce 6–8 wet diapers and 3+ soiled diapers a day. | Pink or red brick dust in diapers. Early diaper counts are an unreliable marker of sufficient vs. insufficient feeding, but fewer than 3 wet and 3 soiled diapers may be signs of insufficient feeding. |
| Feeding behavior | Should be monitored continuously by parents and care providers. |
Signs of a HUNGRY newborn in above infographic Concerns about insufficient feeding should trigger a full evaluation of infant feeding, breastfeeding efficacy, milk supply, and clinical signs of dehydration, weight loss, and laboratory evaluation. |
|
Breast Milk Production |
Manually express before each feed to confirm the presence of colostrum. Breast pumping once lactogenesis II occurs can measure volume per feed and daily milk production when combined with weighted feeds. Pumping is not accurate enough to measure colostrum production. |
Only drops of colostrum. Once lactogenesis II occurs on day 2 or 3, amounts of less than 1–2 ounces per feed or less than the calculated full daily milk requirement, along with signs of infant dissatisfaction, ongoing weight loss or poor weight gain, and/or laboratory evidence of feeding complications. |
|
Ability of Baby to Transfer Milk |
Weighted feeds are useful to measure volume of feeds to baby after lactogenesis II. Before lactogenesis II, clinical signs of infant feeding and satisfaction, hydration, percent weight loss and laboratory data when indicated are the more reliable. LATCH scores and “pauses” during swallowing may be useful in assessing quality of breastfeeding, but does not indicate adequacy of milk supply or rule out insufficient feeding. |
Shallow or painful latch that results in nipple trauma Falling off the breast after less than 10 minutes Once lactogenesis II occurs, weighted feeds of less than 1–2 ounces after the first day, along with signs of infant dissatisfaction, continued weight loss, poor weight gain and/or laboratory evidence of a feeding complication. Some infants that have higher caloric requirements may require more than 2 ounces. |
| Pre-discharge evaluation |
Have confirmed good quality latch and signs of satisfaction with each feed. Weight check, glucose, bilirubin, sodium, ketones, with next day follow up for all infants that are still losing weight. |
Persistent crying and prolonged or frequent (less than every 2 hours) feeds. See above values. |
Feeding the full caloric requirement of an infant is the only way to restore glycogen reserve and stabilize glucose levels if an infant has been underfed. It is superior to correcting glucose levels with oral glucose (or dextrose) alone[4],[10] and is required to wean a hypoglycemic newborn from IV glucose treatment if they have not been receiving enough calories through feeding. Supplementation can be withdrawn when the mother’s milk is sufficient to meet this full requirement.
The current 2021 ABM hypoglycemia guidelines recommends that hypoglycemic newborns with glucose levels between 20–45 mg/dL should be fed as much colostrum from breastfeeding as possible and be supplemented small volumes of banked donor milk or formula, namely 2–10 mL per feed in the first 24 hours and 5–15 mL per feed between 24–48 hours, which is again based on the natural fallacy that a mother’s average colostrum production is the “physiologic” requirement of newborn infants.[11] Their recommendation is based on an inappropriate and unsafe prioritization of supplemental milk avoidance in the setting of a medical emergency.
These small volumes are not based on the known caloric requirements of newborns to prevent starvation and do not provide the calories needed to stabilize glucose levels or protect a hypoglycemic infant’s brain and vital organs. It is also likely to prolong the conditions of low energy availability that causes injury every minute an infant’s brain is exposed. Preventing brain injury with adequate feeding is infinitely more important to an infant’s health and future outcomes than avoiding or minimizing supplemental feedings or maintaining exclusive breastfeeding status.
Oral glucose or 40% dextrose has been shown to be safe and effective in temporarily correcting hypoglycemia but has been found to be less effective at stabilizing blood sugar than formula or banked donor milk.[4] For infants who develop hypoglycemia due to insufficient breast milk or colostrum supply, supplementation is needed to bridge the gap between a mother’s breast milk supply and an infant’s caloric requirement. Furthermore, normalizing a baby’s blood sugar will provide them the energy they need to breastfeed more frequently and effectively, since hypoglycemic babies are typically sleepy, lethargic, and feed poorly.
We urgently need significant changes to hospital protocols, clinical guidelines, and breastfeeding education for both professionals and parents. There is no justification for withholding monitoring and supplemental feedings from newborns who are at risk for preventable and potentially irreversible complications, and we must do better for all infants and their families.
To learn more about this topic, read the Fed Is Best book available on paperback, e-book, and audiobook.
References
- Jeffrey R. Kaiser et al., “Association Between Transient Newborn Hypoglycemia and Fourth-Grade Achievement Test Proficiency: A Population-Based Study,” JAMA Pediatrics 169, no. 10 (October 2015): 913–21, https://doi.org/10.1001/jamapediatrics.2015.1631.
Purnima Samayam et al., “Study of Asymptomatic Hypoglycemia in Full Term Exclusively Breastfed Neonates in First 48 Hours of Life,” Journal of Clinical and Diagnostic Research: JCDR 9, no. 9 (September 2015): SC07-10, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4606303/
Harris, D., Weston, P., Harding, J. “A good breast-feed does not always result in an increase in blood glucose concentration, in hypoglycaemic babies (abstract).” Perinatal Society of Australia and New Zealand Annual Conference; Townsville, Australia. 2016. https://karger.com/neo/article-abstract/115/3/234/231672/Does-a-Good-Quality-Breastfeed-Improve-the-Blood?redirectedFrom=fulltext
Sen, S., Andrews, C., Anderson, E. et al. “Type of feeding provided with dextrose gel impacts hypoglycemia outcomes: comparing donor milk, formula, and breastfeeding.” J Perinatol 40, 1705–1711 (2020). https://doi.org/10.1038/s41372-020-00776-y
Della A. Forster et al., “Advising Women with Diabetes in Pregnancy to Express Breastmilk in Late Pregnancy (Diabetes and Antenatal Milk Expressing [DAME]): A Multicentre, Unblinded, Randomised Controlled Trial,” Lancet (London, England) 389, no. 10085 (June 3, 2017): 2204–13, https://doi.org/10.1016/S0140-6736(17)31373-9.
Sudeepta K. Basu et al., “Hypoglycaemia and Hyperglycaemia Are Associated with Unfavourable Outcome in Infants with Hypoxic Ischaemic Encephalopathy: A Post Hoc Analysis of the CoolCap Study,” Archives of Disease in Childhood. Fetal and Neonatal Edition, August 17, 2015, https://doi.org/10.1136/archdischild-2015-308733.
Christopher J. D. McKinlay et al., “Neonatal Glycemia and Neurodevelopmental Outcomes at 2 Years,” The New England Journal of Medicine 373, no. 16 (October 15, 2015): 1507–18, https://doi.org/10.1056/NEJMoa1504909.
Paul J. Rozance and William W. Hay, “New Approaches to Management of Neonatal Hypoglycemia,” Maternal Health, Neonatology and Perinatology 2 (2016): 3, https://doi.org/10.1186/s40748-016-0031-z.
Christopher J. D. McKinlay et al., “Neonatal Glycemia and Neurodevelopmental Outcomes at 2 Years,” The New England Journal of Medicine 373, no. 16 (October 15, 2015): 1507–18, https://doi.org/10.1056/NEJMoa1504909.
Harris DL, Weston PJ, Signal M, et al. “Dextrose gel for neonatal hypoglycaemia (the Sugar Babies Study): A randomised, double-blind, placebo-controlled trial.” Lancet 2013;382:2077–2083. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(13)61645-1/abstract
Nancy E. Wight et al., “ABM Clinical Protocol #1: Guidelines for Glucose Monitoring and Treatment of Hypoglycemia in Term and Late Preterm Neonates, Revised 2021,” Breastfeeding Medicine, April 7, 2021, bfm.2021.29178.new, https://doi.org/10.1089/bfm.2021.29178.new.