Mothers Describe Their Triple Feeding Experiences and its Mental Health Impact
by Jody Segrave-Daly, RN, IBCLC-Retired and Lynnette Hafken, MA, IBCLC
What Is "Triple Feeding"?
Triple feeding is a commonly prescribed regimen for increasing milk supply. This requires a mother to first feed her baby for 20-30 minutes at the breast, then immediately pump for 15 minutes, and then feed any expressed milk (and/or formula) through a bottle or sometimes even a syringe to her infant, which can take another 10 to 15 minutes. Triple feeding—that is, breastfeeding, supplementing, and pumping every two to three hours—is often prescribed for low milk supply/poor weight gain. Since frequent and thorough milk removal is the best way to increase milk production, this makes sense, right? Sure…if the mother were a machine that never required sleep, food, and down time.
But as a human, sufficient sleep and nutrition are critical to a parent’s mental health, not to mention well-deserved enjoyment of her new baby. While the intention is good—to help parents reach their breastfeeding goals—mothers describe triple feeding as “profoundly exhausting,” “one of the worst times in [their] life,” and “hell on earth.” We have even heard of hospitalizations from psychosis due to insufficient sleep, and from dehydration from not finding the time or energy to drink enough water.
Triple feeding originated in the newborn intensive care unit (NICU) for premature infants who were learning to breastfeed but were unable to empty the breast completely. Any pumped milk could be saved for the next supplemental feeding. In this way, the premature baby was nurtured until he or she was strong enough to only nurse from the breast. This can be sustainable for NICU parents because they have access to nurses and lactation professionals to assist during the triple feeding cycle.
For full-term babies who have trouble removing milk or for moms with low milk supply, triple feeding is similarly recommended by lactation consultants. Unfortunately, some mothers who follow this regimen have little support at home to assist in the triple feeding cycle.
Many mothers have to do all three phases themselves every 2 to 3 hours around the clock from the beginning of the triple feeding cycle. Each cycle can take 50-60 minutes to perform. In addition, there are pump parts to wash up to eight times a day, and sometimes other children to care for.
Triple feeding can easily take up the majority of the day and cause severe sleep deprivation. Many report receiving little guidance on how long to triple feed, how to know if it is effective, and when to stop. As a result, these parents endure the equivalent of caring for triplets (feeding a baby at the breast, “feeding” the pump, then feeding a bottle).
Triple feeding requires a considerable amount of effort and time, and there is little time between feedings for the mother to take care of her own basic needs, such as sleep, eating, and personal hygiene.
“I didn’t eat or drink for days because of the time constraints of triple feeding. By the time my baby was admitted to the hospital on day 5 of life, I lost consciousness and then broke down in the corner of his room from profound exhaustion. I’m a doctor and had done surgical and anesthesia residency. I’m used to sleep deprivation. Those five days were hell on earth. Not only did it not work, but I also unknowingly starved my baby under the care of lactation professionals. They knew I had a breast reduction, but I was told to triple feed without a backup plan. That week of my life lives over and over in my head all the time.”
— Dr. Nicole King
Want to learn more about this topic?
Do you want to learn more about breastfeeding while ensuring safe and adequate feeding?
Dr. Christie and board-certified lactation consultant Lynnette Hafken have just released the online Fed Is Best Breastfeeding Course, where they discuss all the things that you will not hear from a breastfeeding book or class. In it they include secret tips and tricks that you normally have to pay hundreds of dollars to learn about, for the same cost of a hospital breastfeeding class. Click below to get in on the training!
Why is the Triple Feeding Strategy Recommended by Medical and Lactation Professionals?
The common reasons for prescribing triple feeding are:
- Poor latching, lack of sustained suckling, oral anomalies, and insufficient milk removal.
- Delayed onset of full milk production and excessive infant weight loss or failure to gain weight.
- Chronic low milk supply for poor breastfeeding management, hormonal insufficiency, insufficient mammary physiology, and unknown mammary dysfunction.
The Theory Behind Triple Feeding
The theory behind triple feeding is based on the first two rules of lactation management: 1) feed the baby and 2) maximize the milk supply.
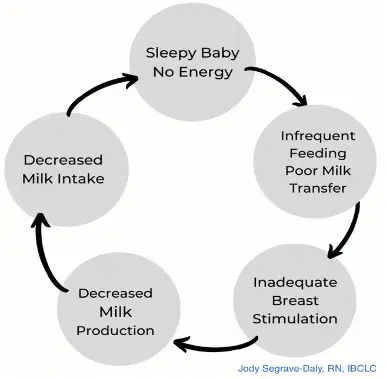
- Maximize removal of breast milk – When a baby is not transferring milk effectively, he is not stimulating his mother’s milk-making hormones adequately, and milk remains in the breast. This causes a reduction in her milk supply and does not provide a full feeding for the baby.
- Give the baby plenty of opportunities to practice and improve latching and sucking – Giving the baby frequent opportunities to breastfeed despite the low milk transfer is thought to help the baby improve his latching and milk transfer skills, and avoids bottle preference.
- Remove more milk through pumping – Pumping after nursing will remove most of the milk from the breasts, thus helping to increase the mother’s milk supply to a sufficient level (a full milk supply is about 25-32 oz/day). When successful, this will allow her to gradually wean the baby from supplementing and return to fully feeding at the breast.
- Make sure the baby is adequately fed – Immediate supplementation is necessary to provide the baby’s full feeding, as babies have caloric, nutritional, and hydration needs that cannot wait until the breast milk supply potentially increases.
Unfortunately, triple feeding has become the default method that is recommended by medical and lactation professionals for a large number of breastfeeding challenges, with no regard to the maternal complications that will eventually occur, or the likelihood of it solving the problem of low milk supply. It is imperative for all mothers to know that triple feeding is not sustainable for longer than four to seven days, and it cannot be recommended unless the mother has a full-time helper. If triple feeding is working, there will be evidence with increased milk supply/volume. This is how we know it is working. If there is no increase, triple feeding will not work for this mother, and her breastfeeding plan will require changes. Most likely it will be a combo-feeding plan.
Before triple-feeding is recommended, your medical and lactation professional must make careful considerations because of the daunting amount of time required to triple feed. The things that need to be considered are:
- Does the mother have full-time in-house help?
- Does she have any preexisting history of mental illness?
- Does she have the best mammary physiology and general health profile to sufficiently increase her milk production? (The word “sufficient” is subjective and is determined by both the baby’s needs and the mother’s goals.)
- Does she have a high-quality electric breast pump?
- Does the proposed triple feeding plan allow for sufficient sleep, nutrition, and self-care to support her basic physiological needs?
Of course, every mother and baby has unique needs and requires individualized breastfeeding management and support. The plan must also be flexible enough to meet unexpected needs.
As part of giving informed consent, it is very important for the health care professional involved to inform parents that they may find themselves unable to follow the triple feeding plan perfectly and that there is no guarantee it will provide the results they are looking for. It is also important to inform parents of the potential impact of triple feeding on their sleep and their physical and mental health.
A backup plan should be provided until changes can be made that the parents are confident they can follow. Lastly, mothers need to know they can stop triple feeding at any given time for any reason. Many will need reassurance and even “permission” to stop triple feeding and to confidently combo-feed or exclusively formula feed, depending on their circumstances, knowing their babies will be healthy and happy as long as they are fully fed with love.
“My lactation consultant recommended supplementing with formula because while I could try to fit in another pumping session for more milk, it’s also important to look after myself. Result: I’m now combo feeding and my baby is thriving.”
—Dina le Roux, mother of Jean-Luc
The Downsides of Triple-Feeding: Mental Health, Bonding, and Accidents
Sleep deprivation from triple feeding has very serious consequences, including postpartum depression, anxiety, psychosis, suicidal thoughts, and deteriorating physical health. Extreme exhaustion has even led to serious accidents when mothers have unintentionally fallen asleep with their babies resulting in infant suffocation and death. Safety must be the top priority of any health recommendation.
Jessica Montgomery talks about how triple feeding stole her ability to enjoy her baby and failed to increase her milk supply.
Literally everything I read about breastfeeding said that undersupply was rare. After she was born, my milk didn’t come in right away. When it did, it was not enough, and she lost weight and had to be re-hospitalized for jaundice, dehydration, and hypoglycemia.
I was willing to do anything to increase my supply and hoped to eventually be able to exclusively breastfeed. I saw two lactation consultants (IBCLCs) and both gave me different versions of the “triple feeding protocol” to try. I was supposed to complete the following three steps every 2-3 hours around the clock:
- Breastfeed baby for at least 10-15 minutes per breast, using breast compressions.
- Supplement baby pumped breast milk, and then formula if pumped milk is not enough. If the baby is able to latch, use a supplemental nursing system, to supplement at the breast, with a tube placed and taped next to my nipple. If she wouldn’t latch, I was supposed to finger feed, cup feed, or use a slow flow bottle.
- Pump for 15-20 minutes with a double pump or for 15-20 minutes on each side if using a single pump. If the baby didn’t empty my breasts I was supposed to do this right away, and if not, I was supposed to wait an hour after nursing to pump.
Triple feeding was my life for months, and my mental health seriously suffered. I couldn’t keep up and that made me feel so guilty, and honestly, it didn’t really do much for my supply. I lost so much time being with and bonding with my baby.
After my second baby was born, I met with a breastfeeding medicine physician who told me that triple feeding was too exhausting for most moms, and it wouldn’t fix my low supply issues because I was diagnosed with insufficient glandular tissue (IGT). I stopped pumping, ditched my SNS, and started combo-feeding my baby. It was amazing for my mental health and literally changed my life.
Bethanne talks about having a psychotic break from severe sleep deprivation while triple feeding her daughter.
I was a first-time mother and was 100% committed to exclusively breastfeeding. She was born at 36 weeks and was very sleepy. She latched poorly, so the LC prescribed triple feeding. I had plenty of help at home and thought everything was going well.
I was profoundly exhausted because I didn’t sleep in the hospital at all. I didn’t recognize my mind was shutting down. I became confused and wasn’t eating or drinking much. I began hallucinating.
My husband called my OB who told him to bring me to the hospital. I was admitted for observation, and the psychiatrist diagnosed me with severe sleep deprivation and anxiety. I had IV fluids and sleep medication and slept for 8 hours straight.
When I woke up, my milk was in, but I was very frail and kept crying. I decided I would become a pumping and formula feeding mother so I could get some sleep. I tell every mother I know not to triple feed because of the hell I lived through. My OB filed a formal complaint against the LC who prescribed triple feeding to me.
How Do We Make Triple-Feeding More Manageable?
Some lactation consultants use a more reasonable model, and here we will describe ours. We prioritize three things:
- sufficient sleep for mother
- sufficient breast emptying to stimulate milk production, and
- sufficient time breastfeeding for the baby to stay familiar with his mother’s breasts as a nice place to be.
As an alternative to triple feeding every 2 to 3 hours around the clock, the following is a modified triple feeding plan that allows a mother to get 5 hours of sleep a night.
Modified Triple Feeding Plan*
- Ensure baby is fully fed to satisfaction at each feeding with breastmilk and/or formula as needed; attempt to finish feeding the baby within 30–40 minutes (you may need to limit breastfeeding time for now).
- Pump after (or instead of) breastfeeding at least every three hours, except . . .
- Get one five-hour block of uninterrupted sleep while someone else does the feeding while you are sleeping.
- Power pump after waking up from the five-hour block of sleep (See Chapter page 216 of the Fed Is Best Book).
- Keep track of your 24-hour milk production to see if the trend increases.
- Determine when the regimen will end—longer than one week of triple feeding can result in severe sleep deprivation that can negatively affect a mother’s health and may not lead to further increases in milk supply.
*No plan is a cookie-cutter strategy that will work for every family. Plans should always be individualized to reflect families’ unique needs and resources. In fact, there is very little in the process of breastfeeding that is the same for everyone!
To save precious time, the baby should only breastfeed when the mother feels up to it and only for as long as the baby is.
Some babies, particularly those who are born early, will sleepily nurse for a long time with just the occasional sucking burst. This is time consuming for moms, and those sleepy sucks don’t do much for the milk supply, which is driven by robust demand (frequent and thorough milk removal). Breast compressions while breastfeeding can also help keep your baby awake and feeding efficiently.
The pump doesn’t get sleepy—it just removes the milk, signaling to the mother’s body to make more. Hands-on pumping (or pumping while massaging the breast to assist expression of milk) [1] provides an extra boost, as does a pumping session when the prolactin levels are highest, between 12 and 5 a.m.
Some mothers find that an at-breast supplementer (SNS) cuts down on time spent feeding. In addition, pumping one breast while feeding at the other, a technique called parallel pumping [2], can also save precious time. This helps some moms while other moms have difficulty coordinating the two activities.
We also want to emphasize the importance of feeding a baby to satisfaction at every feed. This is not only for the baby’s health and comfort, but also to allow him to have the energy to breastfeed well at the next opportunity.
You may hear “the pump is not as effective as the baby” in removing milk, and this statement is overly simplistic and likely incorrect. Research shows that “a healthy breastfeeding infant removes approximately 80% of the total ingested human milk volume in 5 minutes, and an efficient breast pump removes 85% of the available human milk in the breast in 15 minutes.”[3] Whether the baby or the pump is more effective is highly individual based on the mother’s pumping technique, correct flange size, mother’s comfort level with pumping, the type of pump used, and the baby’s skill and energy level for transferring milk.
It is critically important that your plan be flexible and individualized, as some parents have specific needs, for example: insufficient family support, a non-latching baby, difficulty letting down for a breast pump, and/or a history of mental health issues that make sleep deprivation not a safe option. There are countless other infant and maternal factors that require an individualized plan. In some cases, such as insufficient glandular tissue (IGT),[4] triple feeding might not even significantly increase the mother’s supply, leading to false hope, frustration, self-blame, and burnout, and regret.
Triple feeding can work—we have seen it many times—but there is no guarantee an individual’s body will respond strongly to increased stimulation. The closer you are to the time of birth, the more likely it will be to increase.
If the supply does increase, the next step is to transition back to 100% direct breastfeeding (if that is your goal), while making sure your baby continues to eat enough by monitoring weight at least weekly. If you reach a ceiling in your milk production (no increase over a period of 7 days), it is likely that your body has decided that this is the amount of milk it is capable of making for this baby at this time. You still have options, though.
You can investigate further by revisiting your health history and consulting with an endocrinologist or breastfeeding medicine specialist (a doctor who specializes in lactation; many of them do online consults); you can try a different pump, flange size, or pumping schedule (see our section on exclusive pumping for tips); you can make peace with the amount of milk being produced and successfully breastfeed through combo feeding; or wean entirely from breastfeeding if you wish.
Keep in mind that there is always one more thing to try, and it can be easy to spend lots of time, money, and emotional energy on milk production; we recommend keeping in mind what your overall goals are for feeding your baby, and make sure you are on the right path for everyone in the family’s health and happiness.
Mothers Who Used the Modified Triple Feeding Regimen
Here are three examples of patients who used our plan, individualized to their situations (names and some details changed for privacy):
Nancy
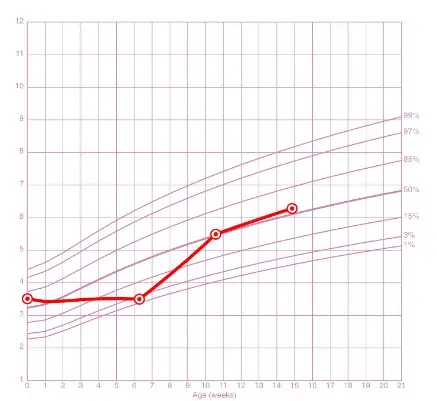
Nancy came to us at six weeks postpartum with her baby still under birth weight. She had been triple feeding for most of those six weeks. Her score on the Edinburgh Postnatal Depression Scale indicated she was probably suffering from severe postpartum depression. Her baby Margot was sleepy and apathetic at the breast, because she did not have the energy to feed vigorously.
Step one was to test weigh the baby before and after breastfeeding. The scale showed Margot transferred 1.5 oz. After this, Nancy pumped 0.5 oz. Two ounces every 3 hours—16 oz/day—was far short of the 25–35 oz needed for healthy infant growth.
Step two was to create a plan that allowed Margot to eat enough to start gaining weight. Once she was fed to satiety with a combination of breastmilk and formula, she started gaining weight appropriately and quickly went from the <2nd to the 50th percentile.
Step three was to ensure Nancy got enough sleep. Initially, dad took over some feedings so Nancy could sleep until she was refreshed, and she power pumped when she woke up. We decided together that she would breastfeed at each feeding for a limited time (Margot would sleepily suckle for an hour if allowed), and pump at least six times a day.
It quickly became clear that Nancy had hit a ceiling on her milk production, and it would not increase beyond about two-thirds of what Margot needed. Margot also started showing signs of frustration at the breast. We then switched the breastfeeding and bottle-feeding around so Margot was bottle-fed until she was relaxed, then breastfed for “dessert” (See page 261 of the Fed Is Best Book). Pumping was gradually discontinued, as it was a source of frustration and sadness. Nancy started seeing a therapist for her postpartum depression, which she attributed largely to the pressure she had put herself under to exclusively breastfeed, and the feelings of anguish that her daughter had gone hungry for six weeks. Margot continued to breastfeed with formula supplementation and then solids until age three.
Pamela
Pamela sought our help at five days postpartum. She was mostly bottle-feeding breastmilk and formula, as her son Thomas would cry and fight at the breast. Her supply was low, estimated at about 12 oz a day. Over the next three days, she followed our modified triple-feeding plan, and her milk supply skyrocketed. Within ten days she was producing a full supply and no more formula was needed. In addition to paying attention to her milk supply, we worked on helping Thomas relearn that the breast was a nice place to be. We recommended that she bottle-feed him skin to skin, and offer the breast occasionally when he seemed willing. We gave him back the control of when he would latch, and as he learned to trust that he would be fully fed at the breast from her now ample supply, he was more and more willing to breastfeed. At about three weeks in, Pamela was exclusively breastfeeding. She chose to continue to have her husband give a bottle in the middle of the night, because that worked well for her family.
Grace
Grace gave birth to her son Ryan at 36 weeks. She had been prescribed triple feeding in the hospital and had dutifully followed it. She said her goal had been to exclusively breastfeed, but now she just wanted to enjoy motherhood rather than feeling angry and resentful all the time. As soon as we talked, I asked her to give the baby to her mother and go to sleep until she woke up naturally. We spoke again when she woke up, and together we developed a plan to increase her milk supply while ensuring she had sufficient time and energy to enjoy her precious baby. Flexibility was the key. Rather than have her pump every three hours during the day, we decided together that she would breastfeed only, and supplement with formula to ensure that Ryan ate sufficient volume. By focusing on direct breastfeeding and eliminating pumping, Grace felt her bond with Ryan strengthening, and her negative feelings faded away. She went on to breastfeed with supplementation for a year.
We Must Do Better for Families
From our experience, triple-feeding regimens that are often prescribed to nursing mothers with low milk supply, though well-intentioned, are inhumane and lead directly to severe sleep deprivation, postpartum depression, and failure to bond. We have seen this over and over. Healing begins when mothers are getting sufficient sleep and are following a plan that allows them to enjoy feeding their babies, while also stimulating their supply according to their goals.
Exclusive breastfeeding is important to some of our clients; we respect their choice to try to maximize their milk supply. For others, the priority is a happy healthy family, and we work with them to achieve this as well.
According to Dr. Marianne Neifert, pediatrician, breastfeeding medicine specialist, and cofounder of the Academy of Breastfeeding Medicine
“The rigors of a triple feeding schedule aren’t for every woman: some are too exhausted or have too many other responsibilities to devote the necessary time and energy to this demanding regimen. If a mom’s emotional well-being is at risk because she keeps trying and trying and it’s still not a rewarding experience, we have to assess whether it’s realistic for her to exclusively breastfeed. Many moms who are having a great deal of trouble and are ready to quit will breastfeed longer if they see it as doable for them.”
“Doable” when it comes to breastfeeding can often mean combination feeding if the milk supply is not increasing or she needs to stop triple feeding.
Maternal mental health must be protected when developing complicated breastfeeding plans. Too many mothers have suffered emotionally because their efforts failed to increase their milk supply. They often conclude that they are failing as mothers and/or failing their baby, which is false.
Mothers need to know that they are more important to their baby and their family than having a full milk supply. A mother’s worth is not measured in ounces. When developing a plan to increase milk supply, health professionals, parents, and their families must work together to protect not only the health and safety of the baby, but also of the nursing parent.
Want to learn more about this topic?
Do you want to learn more about breastfeeding while ensuring safe and adequate feeding?
Dr. Christie and board-certified lactation consultant Lynnette Hafken have just released the online Fed Is Best Breastfeeding Course, where they discuss all the things that you will not hear from a breastfeeding book or class. In it they include secret tips and tricks that you normally have to pay hundreds of dollars to learn about, for the same cost of a hospital breastfeeding class. Click below to get in on the training!
To learn more, order the Fed Is Best book available in print, ebook, and audiobook.
References
- Jane Morton, “Maximizing Milk Production with Hands-On Pumping,” 2017, https://med.stanford.edu/newborns/professional-education/breastfeeding/maximizing-milk-production.html.
- “Here’s How Breastfeeding & Pumping At Once Can Boost Milk Supply,” Romper, accessed August 24, 2021, https://www.romper.com/p/will-breastfeeding-pumping-at-the-same-time-increase-milk-supply-19409301.
- Meier PP, Patel AL, Hoban R, Engstrom JL. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J Perinatol. 2016;36(7):493-499. doi:10.1038/jp.2016.14
- Neifert MR, Seacat JM, Jobe WE. Lactation failure due to insufficient glandular development of the breast. Pediatrics. 1985;76(5):823-828.